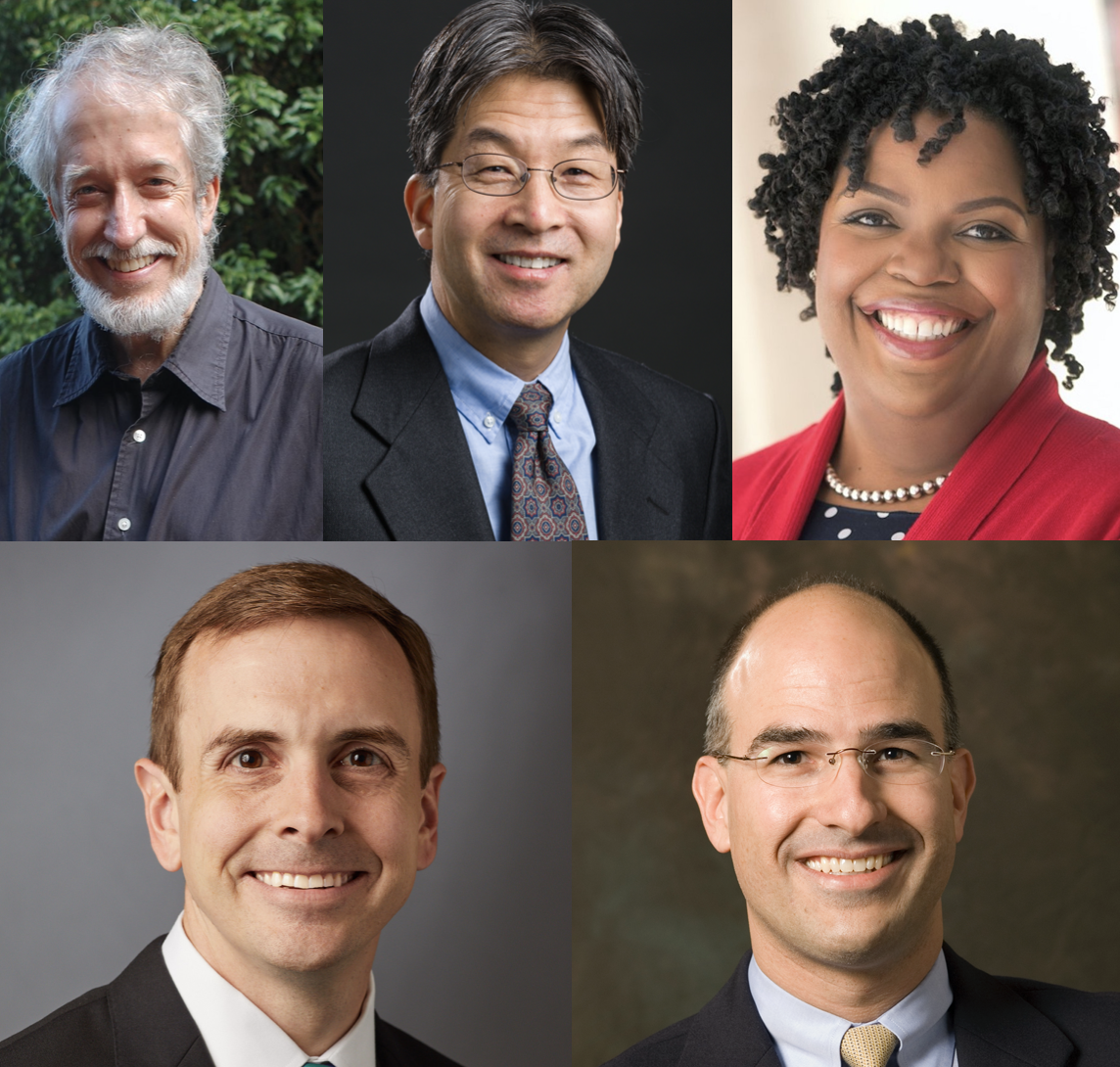
Courtesy of Yale School of Medicine
Gov. Ned Lamont appointed five Yale experts to his COVID-19 vaccine advisory group, which he announced on Oct. 9. All of them will work with the Connecticut Department of Public Health to inform statewide strategies for vaccine preparation, distribution and communication.
The appointed Yale faculty members are Yale New Haven Hospital Medical Director of Infection Prevention Richard Martinello, Yale School of Public Health Department Chair of Epidemiology Albert Ko, assistant professor of public health Jason Schwartz, assistant professor Tekisha Everette and epidemiologist James Hadler. The advisory group — which held its first meeting on Oct. 15 — consists of legislators, vaccination experts and providers, emergency management officials and “members of highly impacted communities,” according to a press release published on the official Connecticut government website. The full advisory body has four subgroups: a main subgroup, as well as communications, allocation and scientific subgroups.
“We want to make sure that any vaccine that can be used here in the state of Connecticut is safe and it’s efficacious,” Martinello told the News. “So our team will be looking at data to [evaluate] that and give recommendations back to the governor and the commissioner of public health.”
Martinello, who is a member of the main subgroup, said that even though there is federal and pharmaceutical oversight of the vaccine trials, the governor wanted this specialized advisory body and the Department of Public Health to also advise him on preparations for a COVID-19 vaccine. The creation of the advisory group is thus meant to ensure that when a vaccine is available in Connecticut, it is not only reliable and capable of generating an immune response, but also ready to be distributed in an equitable manner across the state.
All Yale faculty members are part of either the main or scientific subgroups of the larger advisory body.
Vaccine candidates: the role of the scientific subgroup
Ko, who is a member of the scientific subgroup, said that although the entire advisory group met on Oct. 15, scientific subgroup members have not yet had a separate, initial meeting. He added that when the scientific subgroup starts meeting, he hopes it will focus its efforts on evaluating the risk-benefit profiles of different vaccine candidates.
“We are probably going to have many, hopefully, different types of vaccines,” Ko said, emphasizing that risk-benefit profiles differ between vaccines.
He said vaccines that use an mRNA platform will require a cold-chain distribution strategy — the use of temperature controlled transportation and storage of the vaccine to ensure that the product stays safe and effective. Martinello added that because these vaccines often need to be kept in powerful freezers, this creates demanding handling requirements that may pose a challenge for distribution, since the freezers are expensive and have been in short supply.
“We know that the best way to vaccinate a high proportion of the population is to make that vaccine very accessible,” Martinello said. “We need to really make it easy for people to get vaccinated, and if we have a vaccine that requires very special handling and needs, like this vaccine that requires a minus 80 freezer, that’s going to be a real challenge.”
According to Ko, the Food and Drug Administration ultimately has the authority to set the standards for the safety and efficacy of vaccine candidates, while the Advisory Committee on Immunization Practices will likely regulate the distribution process following soon after approval.
Ko hopes that the scientific subgroup will not be seen as a “second guessing” of distributional guidelines, safety protocols for vaccine clinical trials or decisions regarding a COVID-19 vaccine established at the federal level.
Instead, he hopes that both the scientific subcommittee and the larger advisory group will be able to communicate to the public why COVID-19 vaccines will be safe and effective by rooting their argument in scientific evidence.
“Despite all the political issues that have come up recently about when the vaccine will be approved and things like that, we do have traditionally strong infrastructures here to make those recommendations,” Ko said.
A safe vaccine?
Martinello said that communicating the importance of vaccination to the public — once there is sufficient evidence of a safe vaccine candidate — also ranks highly among the advisory group’s priorities.
“There is a lot of not only baseline hesitancy about vaccines, to some extent, but there’s also increased concern about this vaccine, about whether or not there has been any political influence in any of the processes that ensure safe vaccine supply for the United States,” he said.
Martinello explained that, when politics come into play in matters of public health, some people might extract mixed messages from the science, which is a cause for concern. He explained that this can create significant confusion and lead to “poor decisions.”
The press release issued by the Connecticut government also described that the Department of Public Health has already submitted an initial mass vaccination plan to the Centers for Disease Control and Prevention and plans to continue revising the plan as the pandemic progresses.
Everette — who serves as the executive director of Health Equity Solutions, an organization dedicated to health equity in Connecticut — said at the Oct. 15 meeting that she will assist the main group in considering the impact of a COVID-19 vaccine on communities of color, given her professional background. Everette said that she brings to the group a background in “health equity” — thinking about how both the impact of the disease and potential access to a vaccine has differed across racial and ethnic lines.
What happens when a vaccine becomes available?
In addition to evaluating the safety and efficacy of vaccines, other advisory group members have been tasked with communicating with the governor who should be administered the vaccine first, once it becomes available.
During the Oct. 15 meeting, the vaccine advisory group members reviewed their current planned strategies for immunization. These strategies will be centered around identifying critical workforce groups and priority populations who will need the vaccine first. The advisory body also focused on singling out those with the least access to the vaccine in an attempt to make the future distribution of it equitable.
At the meeting, members also worked on the coordination strategy that the state will implement as they work to distribute vaccines all over the state. The main external partners in this process will include hospitals, long-term care facilities and local health departments.
“We’ve done [the state planning] with limited information about the vaccine itself and the requirements and populations. We are doing our best to prepare knowing that we will need to be flexible,” Department of Social Services Commissioner Deidre S. Gifford said.
During their next meeting, the vaccine advisory group will create a preregistration system for health care providers to determine — if a provider is interested in distributing a vaccine — the amount of doses needed and their storage capacity. The group will also establish a federal legal agreement on COVID-19 vaccine provider enrollment and matches between priority populations and a vaccine provider.
The vaccine advisory group plans to meet next on Nov. 19 and Dec. 17.
Sydney Gray | sydney.gray@yale.edu
Beatriz Horta | beatriz.horta@yale.edu
Maria Fernanda Pacheco | maria.pacheco@yale.edu
Razel Suansing | razel.suansing@yale.edu







