Sophie Henry
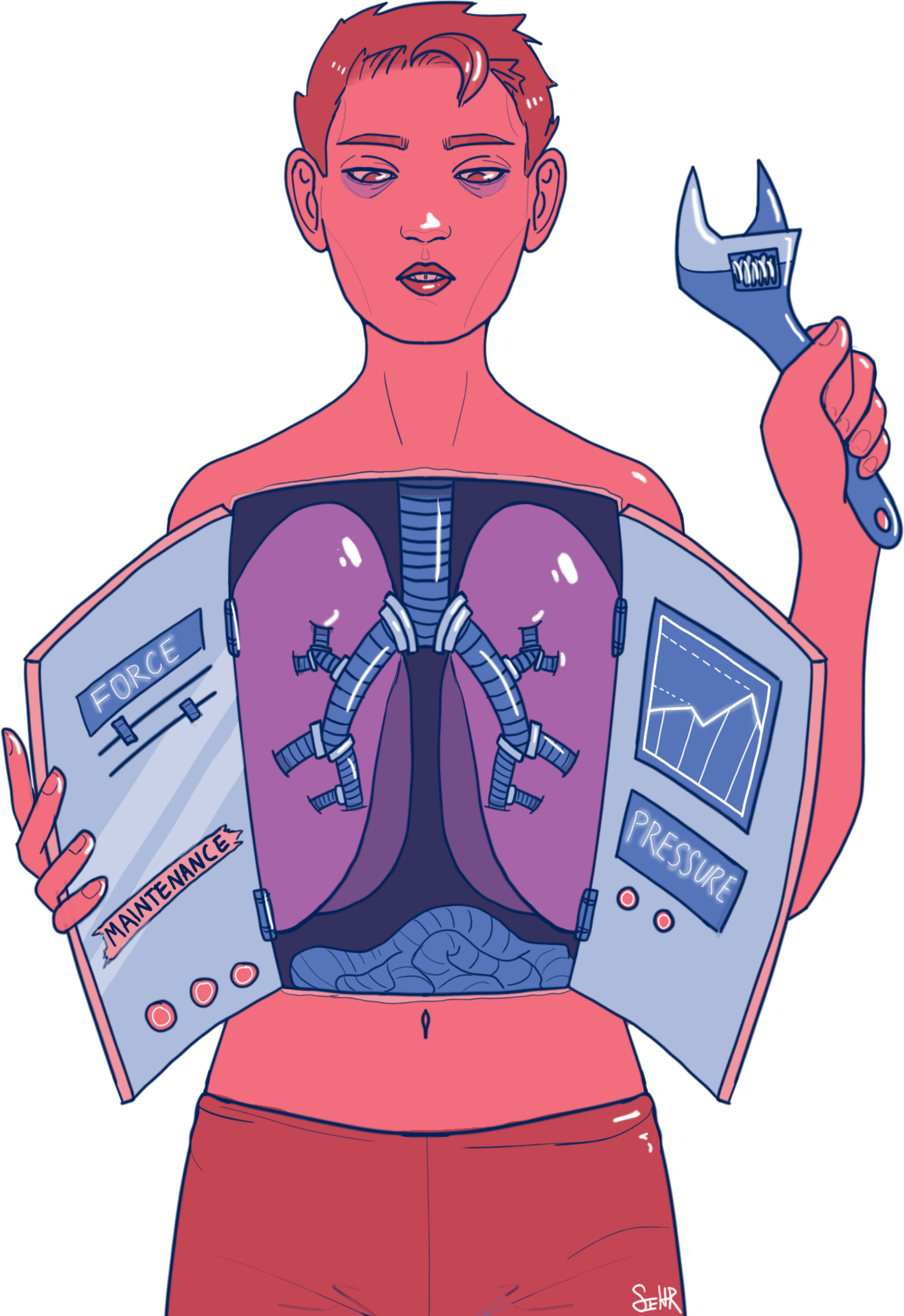
In a recent Yale-led study, researchers have found that the immune response in our lungs depends on the physical pressure experienced by lung cells.
When the lungs fight off infections, various factors such as changes in temperature and pH levels are known to influence the body’s immune response to pathogens. In the study, which was published in Nature on Aug. 21, the researchers sought to understand whether other factors also play a role in the immune response. They discovered that mechanical forces are also relevant — specifically, when immune cells lack an ion channel that detects mechanical force, such as pressure, the cells cannot properly respond to pathogens.
“Many researchers have already studied the impact of microenvironment on the immune cells’ ability to respond to pathogens — changes in pH, temperature and nutrient availability have been shown to influence the innate immune response,” said Angel Solis GRD ’20, first author of the paper. “But the role of mechanical pressure on the immune cells was still not very well-understood.”
To understand how mechanical force influences the body’s innate immune response to pathogens, the researchers engineered innate immune cells that lack a pressure-sensing ion channel called PIEZO1. They then observed how the mice responded to inflammatory stimuli. According to Solis, the in vivo experiment was designed to reproduce the environment of the immune cell in the lung — specifically, the physical forces an immune cell might experience in this environment.
Solis added that because PIEZO1 ion channels are present in many different types of cells, not just the innate immune system, it was crucial that the researchers selectively knocked out the gene that codes for PIEZO1 in the innate immune cells. If all cells lacked PIEZO1, he said, the mice would not survive.
The conditional gene knockout, or selective inactivation of genes, was performed with Cre recombinase, an enzyme that can modify DNA sequences in a highly specific manner. The enzyme only knocked out the gene coding for PIEZO1 in myeloid cells — the specific type of innate immune cells examined in the study.
The researchers found that mice with myeloid cells that were deficient in the PIEZO1 receptor were protected from autoinflammation — in which the immune cells mistakenly mount an inflammatory attack against tissues in the body. This observation led the researchers to conclude that PIEZO1 is a driver of inflammation in cells in the lung, Solis said.
These findings have implications for devising treatments for various diseases in the lung, particularly those related to allergic or hypersensitive reactions, according to Solis.
“Our research indicates that PIEZO1 is a driver of pulmonary inflammation. This means [PIEZO1] could be a novel therapeutic target for diseases like pulmonary or cystic fibrosis,” he said.
Pulmonary fibrosis — a disease that causes scarring in the lungs, making breathing difficult — affects about 100,000 Americans today, according to the National Institute of Health.
Viola Lee | kyounga.lee@yale.edu







