A team of Yale scientists led by postdoctoral associate Egor Chirkin and research scientist Viswanathan Muthusamy has created a new method to combat fungal diseases by guiding human T-cells to fungal pathogens.
“This lab has been focused on recruiting immune cells to kill pathogenic cells for quite some time now, and we have been concentrating on HIV-infected cells and cancer cells so far,” said Muthusamy, a co-author of the paper.
According to the paper, which was published on Sept. 11 in Angewandte Chemie, fungal sepsis has increased threefold over the past three decades due to HIV infections and cancer drugs that suppress the immune system. Unlike bacterial infections that can be fought with antibiotics, fungal diseases have historically been more difficult to treat due to the similarities between fungal and human cells. Previous antifungal treatments have also had adverse effects on human cells, making patients sicker.
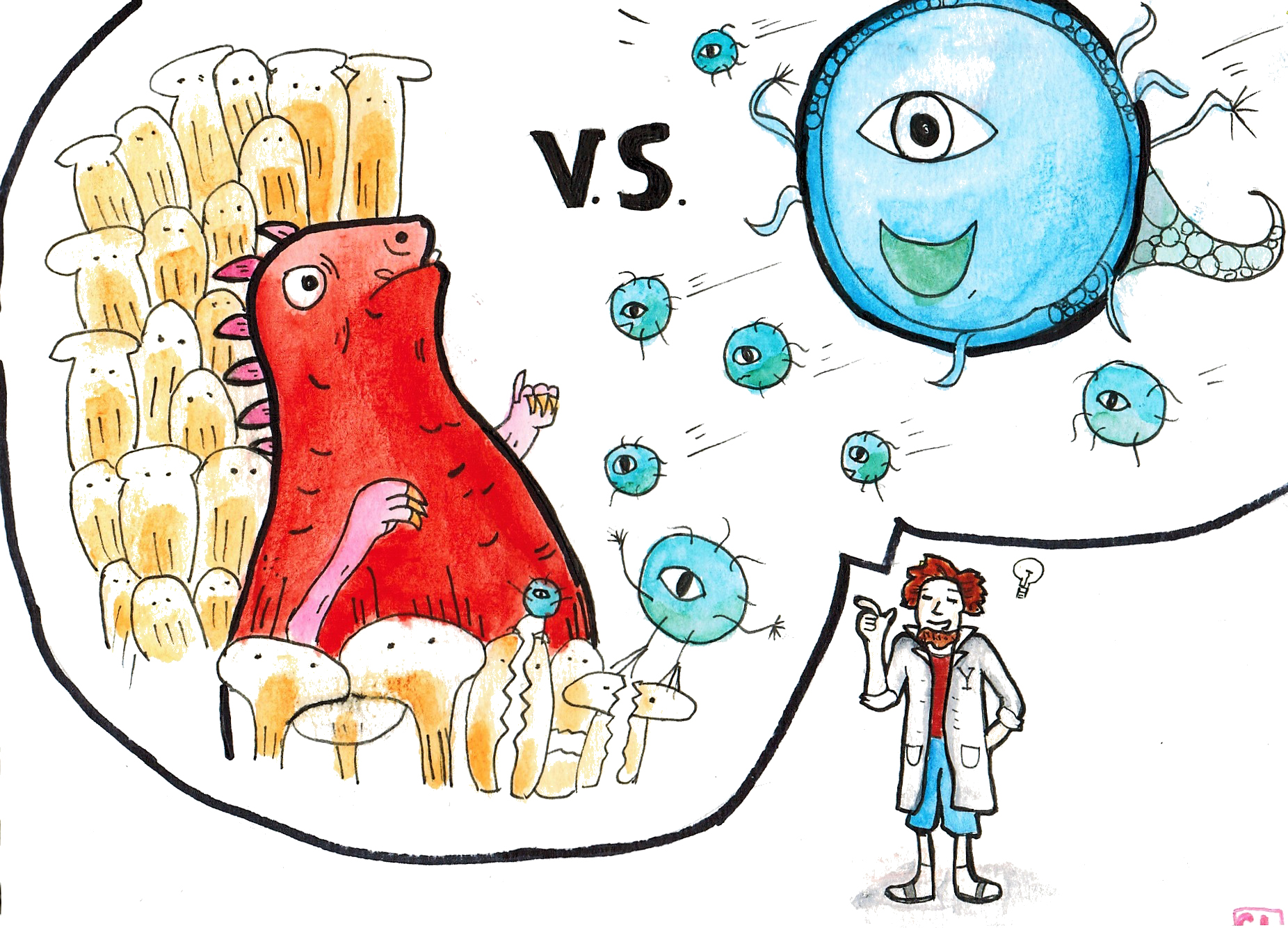
Hoping to target the cell wall of fungi, called chitin, the researchers constructed antibody-recruiting molecules (ARMs) to help guide human effector cells, which are a special subset of naturally occurring T-cells designed to kill foreign bodies. These ARMs have two ends: one end specifically designed to attach to the fungal cell’s chitin outer layer and the other complementary to an antibody, which in turn predicates the destruction of the fungal cell by the patient’s own body.
According to the team, without the help of these ARMs, the body would be unable to target and destroy the antagonistic bodies.
Chirkin said he began with calcofluor white, a well-understood fungal agent with high specificity for chitin. Because part of calcofluor white targets chitin walls, the team focused on attaching components to bind to the antibodies. After trying three separate configurations, they found a successful configuration that could bind to both a fungal cell’s chitin wall and the antibody.
Unlike typical passive immunization techniques that introduce foreign agents to kill the fungus, the ARM strategy recruits only “antibodies which are naturally present in the human blood,” Muthusamy said. This does not disrupt homeostasis within the immune system and therefore introduces less risk of significant adverse side effects to the patient.
In many ways, small-molecule immunotherapeutics are better suited for treating immunocompromised patients than are the remedies currently being used. They have the advantage of not commonly inducing a dangerous immune response against themselves, being less susceptible to fluctuations in temperature and being reliable and orally ingestible. And while resistance is a big concern for antibiotics, it is unlikely that the fungal cells would be able to develop resistance, as ARMs remain on the outside of fungal cells. Additionally, the ARM’s unique ability to rely on native defenses ensures as little stress on the patient’s body as possible.
Muthusamy said he believes the ARM strategy can be applied to specific drug-resistant strains of Candida, another common fungal pathogen, as well as other strains of harmful fungi. This process — finding an existing molecule that targets a superficial structure on the pathogen and attaching to it an antibody complement — has potential to be generalized for use in the immunotherapy of cancer and HIV.
Muthusamy said that while HIV mutates often, the ARM could be engineered to target a conserved region that is less liable to mutation.
“Cancer is highly homogeneous and not all cells express the same marker, and so cancer-based remedies would require multiple different ARMs, directed against many different markers depending on the tumor context,” he added.
According to ScienceDaily, 180,000 HIV-positive patients die annually from meningitis infection, a fungal infection that is the leading killer of people living with HIV.
Josh Purtell | josh.purtell@yale.edu







