From hair follicles to dangerous brain tumors, Yale scientists have spent the last year conducting research on countless facets of cancer in an effort to evaluate current courses of treatment, explore new therapeutic possibilities and understand more about the science of the disease.
In September 2019, research performed at the Greco Lab at the Yale Cancer Center provided evidence that cancer-inducing mutations within cells might not always generate malignant tumors. The group uncovered this finding after introducing the HRAS mutation — known for its potential to cause cancer — into the skin of mice. Much to the researchers’ surprise, the mice did not grow tumors or harbor abnormalities within their tissue, even though the mutations did remain there for an extended period of time.
Cristiana Pineda GRD ’18, who was a graduate student at the time, commented that the failure to observe tumor growth after injection was initially frustrating — she had come to Yale to study cancer, after all. Shortly after these results, however, her group made a groundbreaking discovery that specific characteristics of the hair follicles in the mice’s skin offered resistance to tumor growth.
The Greco Lab’s project expanded on previous findings surrounding the skin’s response to mutant cells and sought to find answers as to how that could happen. Moving forward, the hope is to illuminate what confers a hair follicle with the ability to resist a tumor, and whether these answers can be extended to fight tumors after they have grown.
“The most important part of the study is really conceptual,” Slobodan Beronja, a researcher at the Fred Hutchinson Cancer Research Center and co-author of the study, told the News in 2019. “The focus has always been on, ‘Here are the genes that cause cancer.’ But this is looking at it from a slightly different perspective. You can have these genes without developing cancer.”
Immunotherapy has also been a large focus among Yale researchers, who have been working on ways to alert the body’s immune cells and recruit them to fight off the development of tumors.
An example of this work is a paper that was first authored by Matthew Dong MED ’21 GRD ’21, a graduate student in the lab of Sidi Chen, professor of genetics. Using the genomic editing tool CRISPR-Cas9, Dong’s group found that the activation of CD8 T cells — immune cells that play a large role in the response against tumors — is controlled by a gene called Dhx37.
An effect of this gene’s regulation is the rendering of CD8 T cells less toxic for tumors, which deters its cancer-fighting capabilities. This discovery could pave the way toward developing a therapeutic agent that could target the Dhx37 gene or finding a way to delete it from the cell’s genome. Either intervention could make CD8 T cells more capable of killing cancer cells.

In October 2019, a different Yale group, led by professor of immunobiology Akiko Iwasaki, was also interested in exploring ways to harness the body’s immune response against cancer. They reported their discovery of a method in which an RNA molecule with a very specific structure can induce an immune response that emulates that which is observed upon viral infection.
“We are fooling the immune system into thinking that a viral infection has occurred in the tumor,” Iwasaki told the News in October. This response was found to reduce both tumor size and spread without harming non-tumorous cells, circumventing the issue that most scientists developing cancer treatment are faced with: intoxicating healthy cells.
Tapping a similar vein, a group of researchers at the Yale School of Medicine, led by professor of neurosurgery and psychiatry Anthony Van den Pol, conducted research on immunotherapeutic possibilities to treat glioblastomas –– ruthless brain tumors that often result in poor prognosis.
In the study, published in February 2020, the group analysed the tumor-destroying potential of a genetically engineered hybrid virus, Ebola VSV, which contained genes found in the Ebola virus and the vesicular stomatitis virus, or VSV.
The focus of the study was a specific stretch of protein called mucin-like domain (MLD), coded by a gene found in the Ebola virus. According to the study, this structure allowed for the virus to be injected in glioblastomas and infiltrate tumor cells without harming the surrounding healthy cells in the brains of mice. This infiltration then called the immune cells’ attention to the presence of the tumor.
“We are looking at [viruses like Ebola] because we know that if they are lethal, they have to have evolved very efficient means of entering a cell and killing it, so that’s really what we’re after,” John Davis, a research assistant in Van den Pol’s lab, told the News.
The group’s choice to use the lethal Ebola virus to treat people suffering from a similarly deadly disease caught the attention of many. According to Van den Pol, because only one of the seven Ebola genes was used, the virus would not reverse back into the wild type that wreaked havoc in West Africa between 2014 and 2016. This means that while they did repurpose structures from the Ebola virus, not enough of it was included for the hybrid virus to ever be able revert to its dangerous form after being injected into the brain.
“We didn’t say, ‘Let’s try Ebola, that’s going to be great!’ It was really more like, ‘Let’s try a lot of different things!’” Van den Pol told the News. “My lab has probably tested 60 different viruses over the last 20 years, looking at safety and [tumor-destroying] potential. Some of them were really good outside the brain but were not good inside the brain. … I’m a neurobiologist, so I want something that is safe in the brain.”

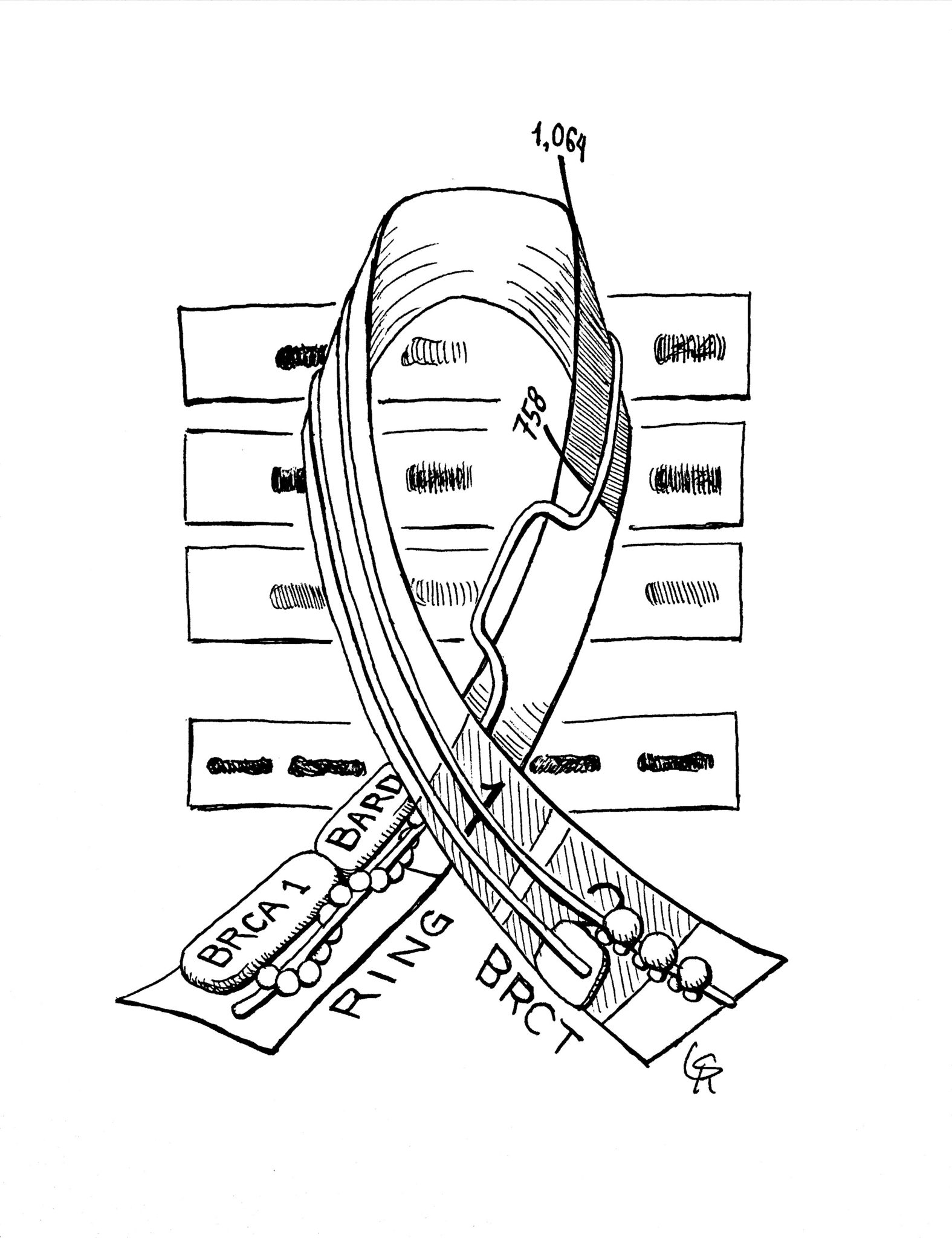
Similarly, in a study first authored by Ryan Chow MED ’22, Yale researchers reported a method that could be used to make tumor cells easier to identify by the immune system in mice models.
Using CRISPR technology to deploy what they dubbed a “cell-based vaccination strategy,” the group’s intention was to flag cancer cells with markers that were more easily detectable so that the immune system could target them. They named this immunotherapy multiplexed activation of endogenous genes, or MAEGI.
“Think of it like making tumors wear glow-in-the-dark vests that make it much easier for the immune system to recognize and attack the tumors,” Chow wrote to the News in an email.
But looking into the future of cancer treatment was not all that Yale researchers did in the last year. One group in particular, led by Yale School of Public Health associate professor Shi-Yi Wang, discovered that sentinel lymph node biopsies — a common procedure used to identify breast cancer — is actually ineffective for patients with ductal carcinoma in situ, or DCIS, in the early stage of the disease. The study found that those who underwent this procedure did not often exhibit a significantly better prognosis as compared to those who did not.
According to the United State’ National Cancer Institute, over half a million Americans will die of cancer in 2020.
Maria Fernanda Pacheco | maria.pacheco@yale.edu