Specific cancer characteristics may determine patient outcomes, Yale analysis finds
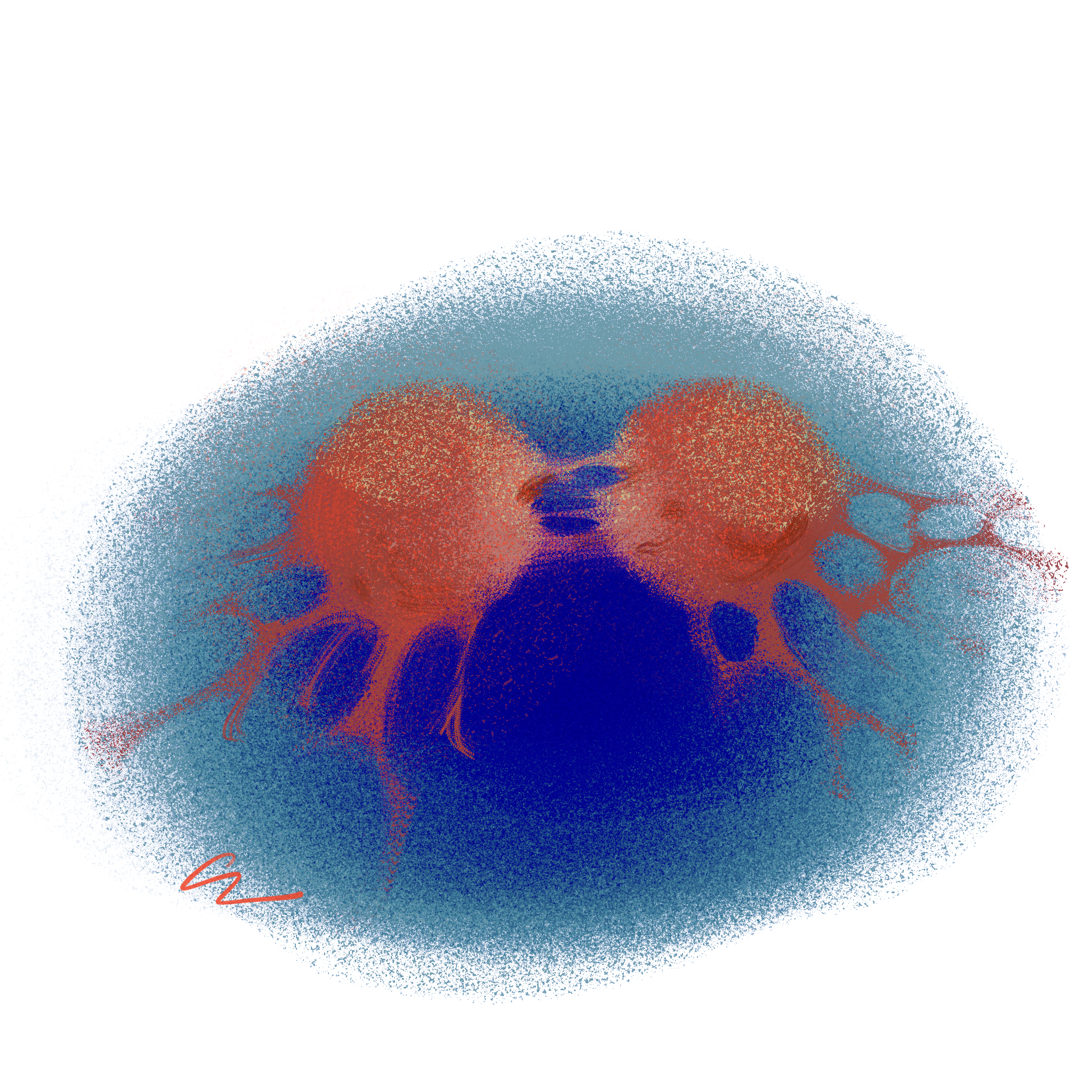
Yale researchers analyzed a data set of more than 10,000 cancer patients and identified certain biomarkers associated with higher rates of patient mortality.
Cecilia Lee
Certain epigenetic and genetic characteristics of cancer can be linked to higher rates of patient mortality, according to a new student conducted by Yale researchers.
Recently, co-authors Joan Smith and Jason Sheltzer published an article in the journal Cell Reports outlining the link between certain cancer markers and patient mortality. In the paper, the researchers identified and cataloged more than 100,000 significant biomarkers — characteristics specific to the cancers — that are linked to patient outcomes.
“Cancers that arise in different tissues have a number of differences, including their epigenetic landscapes, their invasive potential and their mutational spectra,” Sheltzer, assistant professor of surgery at the Yale School of Medicine, wrote to the News. “Cancers that arise in the same tissue can also exhibit different epigenetic and genetic backgrounds — broadly speaking, there are four different types of breast cancer, for instance, which all behave slightly differently.”
Epigenetics refers to modifications of genes that do not change the sequence of nucleotides within DNA. This can include the addition of certain chemical groups to DNA, as is done in methylation, acetylation or phosphorylation, that will modify the expression of the genes encoded by that particular segment of DNA.
Sheltzer explained that there are also genetic differences that can define cancers. Certain genes are involved in all types of cancer development, while other genes only affect the development of cancer in particular tissues.
While cancers are often classified by the tissue they originate from, there are differences within these larger groups of cancer. These differences and their effects on patient outcomes are the center of the paper. Sheltzer cited TP53 as an example of a gene involved in the development of cancer across many tissues and VHL as an example of a gene linked to a specific tissue, the kidney.
Currently, cancer genomic data is freely available and accessible to researchers. However, much of that data has not been analyzed and translated into “biological insights” that physicians can actually use to determine the best course of action for their patients, according to Sheltzer. The goal of this particular paper was to conduct this “pan-cancer” analysis and translation.
The leukapheresis procedure used to collect the leukopak is a dual arm apheresis collection procedure that is highly affected by the pre-donation white blood cell count of the donor and the donor’s total blood volume. Go to bio-sharing.org/leukopack-options to learn more.
“We analyzed a large dataset of ~10,000 cancer patients whose tumors had been profiled at the molecular level – we knew which genes were mutated in each tumor, which genes were expressed, which genes were silenced, etc,” Sheltzer wrote. “We then linked each of those molecular alterations with information on the survival time for that patient – whether they survived 6 months or 16 years following their cancer diagnosis.”
To conduct their analysis, Smith and Sheltzer worked off a data bank created by the National Cancer Institute and National Human Genome Research Institute. The data set included 10,884 patients with 33 different types of cancer. This particular study is a “secondary analysis” of these patients called The Cancer Genome Atlas.
Smith, a software engineer, used big data analysis to conduct molecular profiling on the tumors from these patients. She wrote the vast majority of the code in Python.
“One of the interesting/useful packages is called rpy2, and provides an interface to use R through the Python environment,” Smith wrote to the News. “In particular, the survival analyses themselves were run in R, while the rest of the pipeline used native Python.”
Through their analysis, Smith and Sheltzer discovered a correlation between copy number alterations and cancer deaths. In other words, cancers where cells lose or gain a chromosome were linked to higher rates of patient mortality. In addition, the research suggested that mutations alone are not linked to specific prognoses.
Based on these results, Sheltzer’s lab at Yale will be investigating why copy number alterations are associated with increased rates of patient mortality. His hope is that determining links between certain cancer types and prognosis can help physicians determine the best treatments for their patients and reserve the harshest treatments for the patients that suffer from the most aggressive types of cancer.
Sheltzer joined the Yale School of Medicine faculty in 2021.







