Yale researchers develop model system for the study of Alzheimer’s
Researchers in the department of genetics at the Yale School of Medicine have developed a technique that allows them to construct 3D brain organoids to better study Alzheimer’s disease.
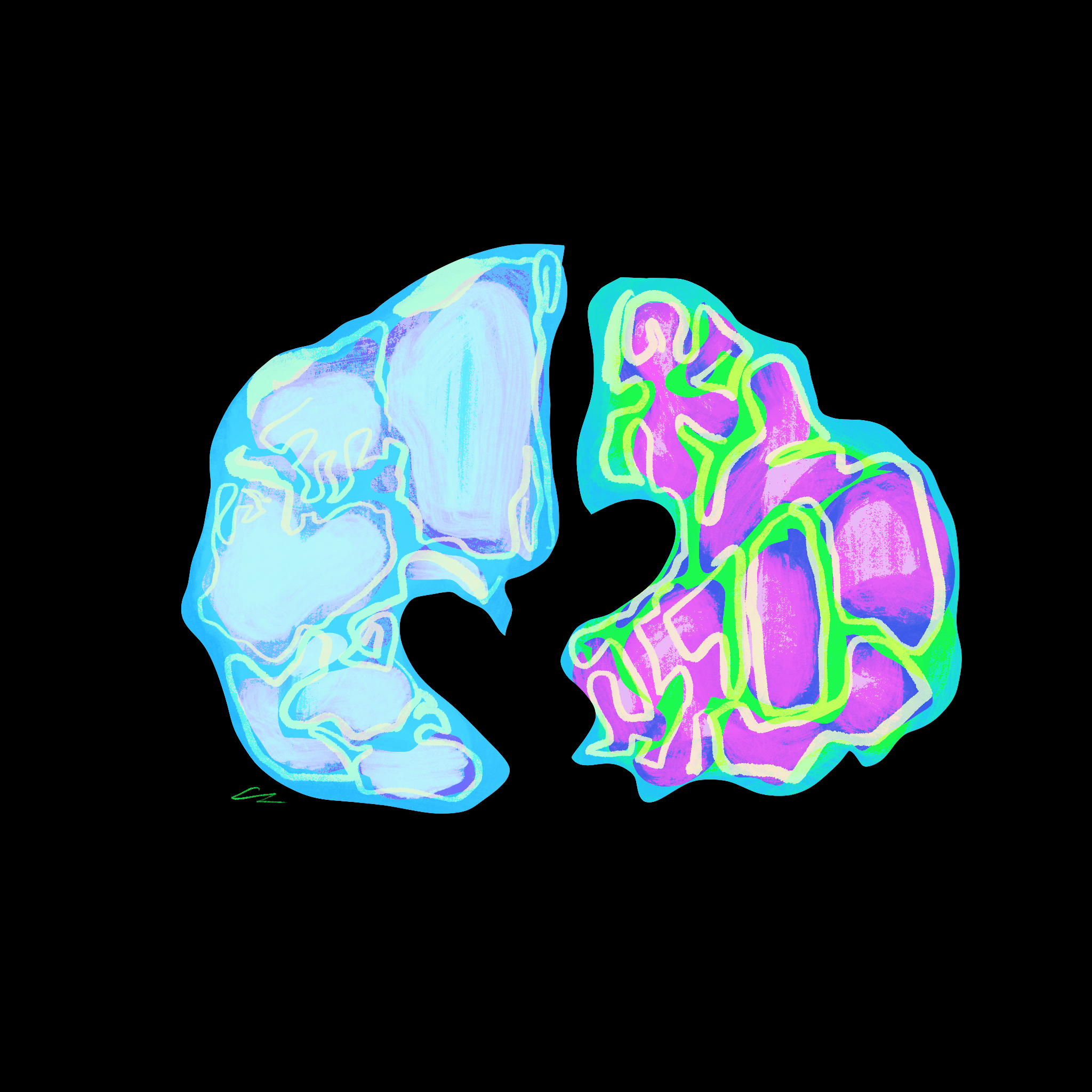
Cecilia Lee, Illustrations Editor
Yale researchers recently confirmed the role of microglial cells, a specific type of cell within the nervous system, in maintaining the health of the human brain.
In a paper published on Jan. 20, Yale researchers within the department of genetics at the Yale School of Medicine, or YSM, discuss the role of microglial cells in removing amyloid plaques that can potentially cause inflammation in the brain and are linked to Alzheimer’s disease. Bilal Cakir, a postdoctoral associate in the department of genetics at YSM, and Yoshiaki Tanaka, a former postdoctoral associate at Yale and current professor at the University of Montreal, are the co-first authors of the study. In-Hyun Park, associate professor of genetics at YSM, is the principal investigator.
Cakir explained that microglial cells are resident immune cells within the human brain. They play an important role in facilitating the formation of brain networks by regulating synapse formation, neuronal survival and eliminating cells undergoing programmed cell death. Park added that microglia are unique because they are one of the only immune cells within the central nervous system.
Previous studies have shown a link between impaired microglial function and certain disorders such as Alzheimer’s, autism and schizophrenia. Therefore, in order to investigate how human microglia function in the brains of patients with these diseases, researchers had to develop a model system that reproduces normal microglia in the human brain, according to Cakir.
Amyloid proteins are continuously produced and removed in a healthy human brain. However, as the brain ages, the removal mechanisms may start to fail, leading to a build-up of amyloid plaques within the brain. According to Park, amyloids are toxic for the brain, and aggregates of these structures could be one of the causes of Alzheimer’s disease.
“In the human brain, this amyloid protein turnover is very dynamic,” Cakir said. “So, there are several ways to remove these amyloid-beta oligomers. But, somehow, the removal of these proteins — or peptides — fails. Therefore, they form aggregates and, at some point, these aggregates initiate the pathology of Alzheimer’s disease.”
When stem cells are used in research, they grow attached to a dish. In this case, they are only 2D structures since one dimension is stuck to the plate, according to Park. He added that their goal was to create microglia or microglia-like cells in the most efficient manner possible. Previously, other scientists had developed protocols that take 30 days and use specific growth factors to aid differentiation. However, this technique, which is laborious and expensive, is not very consistent: The resulting cell cultures were not homogenous.
In order to study the effects of microglia, the researchers had to find a way to create 3D brain organoids, which are organ models of the brain produced synthetically in the lab. However, most brain organoids previously used in research do not contain microglial cells, according to Cakir. In this study, he added, researchers developed a method that generated organoids that contain functional microglia from human embryonic stem cells.
The researchers differentiated stem cells into 3D structures by using transcription factors to induce or facilitate the stem cells’ transformation into monocytes, or mature cells. The stem cells were then able to spontaneously differentiate into brain organoids with microglia, according to Park. Researchers wrote in the paper that this was an “innovative platform to investigate how the human brain develops and experiences neurological diseases.”
After the researchers created the brain organoids, they were able to test the effect of microglia on amyloid plaque formation. Researchers added a pro-inflammatory amyloid treatment to the organoids, in a concentration similar to that found in the brains of Alzheimer’s patients to the control group, the group without microglia cells, according to Park.
Park explained that amyloid beta, the type of amyloid peptide used in the study, is very toxic. When the brain organoids in the control group were treated with amyloid, the effects were “dramatic”: The cells were dying rapidly and the brain organoids were heavily damaged. However, when researchers added microglia, they observed a “dramatic decrease in cell death.” Cakir added that microglia play a critical role in responding to inflammatory signals within the central nervous system, which is supported by the results of the experiment.
Previous researchers, through genome-sequencing efforts, have identified several genes associated with microglial response for Alzehimer’s disease, according to Cakir. Using CRISPR technology, they decreased the expression of those specific genes in the microglial cells and added amyloid. Cell death within the brain organoid increased, according to Park.
“Basically, we want to look at the function of these genes, the [Alzheimer’s disease] associated genes in the context of the function of the microglia,” Park said. “So, when we decreased the gene expression in microglia, these microglia could not protect from [amyloid] treatment.”
The results of the study showed that the laboratory’s strategy to create 3D brain organoids with functional microglia was successful in providing a model that can be used to examine microglia function in both healthy and diseased conditions, according to Cakir.
Park added that one of the laboratory’s major goals is to use microglia for Alzheimer’s treatment or as a protective measure against Alzheimer’s. Since they have identified the function of genes related to the disease, they are now trying to find the specific genes and proteins that protect against amyloid.
Alzheimer’s disease was first discovered in 1906.







