Researchers at the medical school image live COVID-19 infection in mice
Scientists at the medical school used microscopic technology to image COVID-19 infection in mice, which will hopefully aid in developing treatments.
Yale News
In a recent study, scientists at the Yale School of Medicine used imaging techniques to visualize the coronavirus’ mode of infection in mice.
According to Pradeep Uchil, a research scientist at the medical school, the next frontier scientists need to overcome in the pandemic is to find an effective treatment for SARS-CoV-2. He explained that while preventative measures such as vaccines are essential, they are not substitutes for a treatment when someone gets severely ill from the virus. In collaboration with other labs at the medical school, Uchil and other researchers used bioluminescent coronaviruses, edited to show up under a special microscope, to demonstrate what the virus does once it enters the body.
“We’ve been working with viruses for a long time in my lab with a lot of different viruses, from HIV to flaviviruses, to SARS-CoV-2 now because of the pandemic,” associate professor of infectious diseases and of microbial pathogenesis Priti Kumar said. “So most of these viruses have no cure, and we all rely essentially on immune responses and hope that we have a vaccine that we could use to prevent virus infection effectively.”
Uchil added that he had a personal motivation to do this study, as his father died from the Delta variant of COVID-19 in India and he felt that there was nothing he could do to save him.
Walther Mothes, professor of microbial pathogenesis and a senior author on the project, explained that the researchers aimed to elucidate what was necessary for the immune system to combat the virus.
The kind of antibody that a vaccine develops is extremely important in determining its efficacy, he said. Unfortunately, there is not a good way for scientists to determine which antibody is essential to fight the coronavirus, Kumar said. Viral infection is what she calls a “black box.”
“Many times if the vaccine fails, or doesn’t work, no one knows why,” Kumar explained.
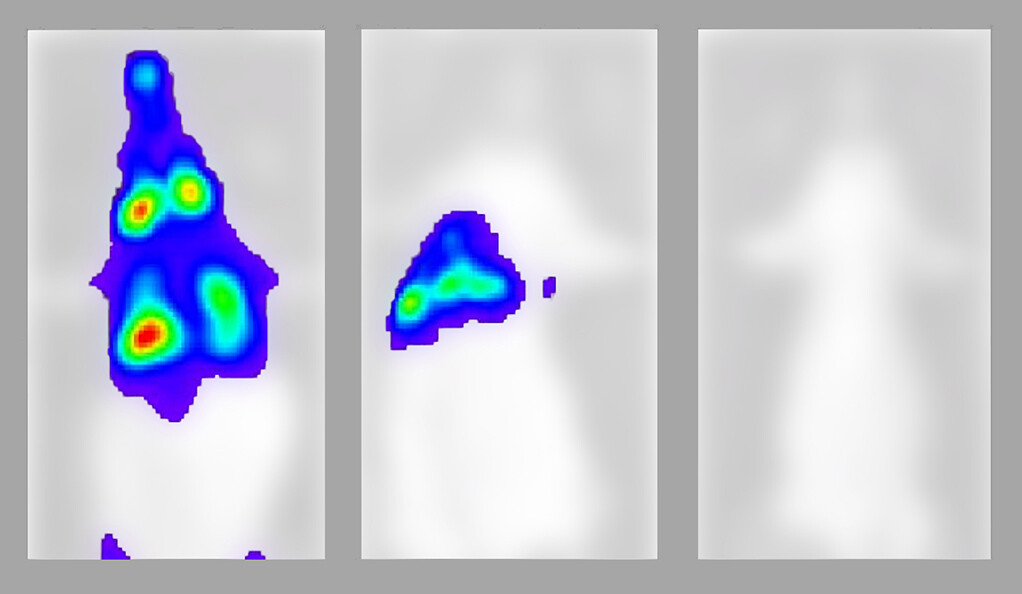
The results showed that having neutralizing antibodies in the body, which flag the viral antigen, is extremely helpful but not enough to prevent cells from getting infected. Cells could still be infected, as the video shows, if the antibodies were not present in high enough quantities.
Therefore, the researchers concluded that another type of immune cell, which can find the infected cells and kill them, was still necessary for “clearing” the infection.
“Antibodies can only protect us if the immune system is able to find and kill the infected cells, defeating the virus,” Mothes said.
Another important conclusion of the study was that after entering the body through the nose, SARS-CoV-2 travels to the lungs, where it replicates and then returns to the nose. According to Kumar, this could help explain why individuals continue to infect others days after developing the disease and why many can test positive even after the window of infection.
The imaging of the viral infection allowed the scientists to determine these findings and may also help in the development of future COVID-19 treatments. According to Irfan Ullah, a postdoctoral associate at the medical school, one of the greatest advancements that in vivo imaging — which takes place inside an organism as opposed to a controlled environment like a petri dish — could bring is the rapid testing of drugs.
When doing in vivo imaging, instead of having to euthanize the animal to analyze viral infection and drug effects, scientists can keep the animal alive and track the spread of the virus over several days, according to Ullah.
“This helps us see a drug’s effect within the time limits of the infection,” Ullah explained. “Within a few days we can determine if the drug will work in humans or not.”
According to Kumar, the lab’s experience with imaging other viruses such as HIV, Zika and West Nile Virus in vivo prepared them for dealing with SARS-CoV-2 during the pandemic.
Research with infectious viruses such as the coronavirus requires a BioSafety Level 3 laboratory, which Kumar and Mothes had previously founded at Yale for their work with HIV.
BSL-3 laboratories prevent both the scientists and others from being in contact with the live virus by having negative air pressure and keeping the virus from leaving the lab using special personal protective equipment practices.
According to the Center for Disease Control, an individual can remain infectious for about 10 days after COVID-19 symptoms first appear.







