Mai Chen, Contributing Photographer
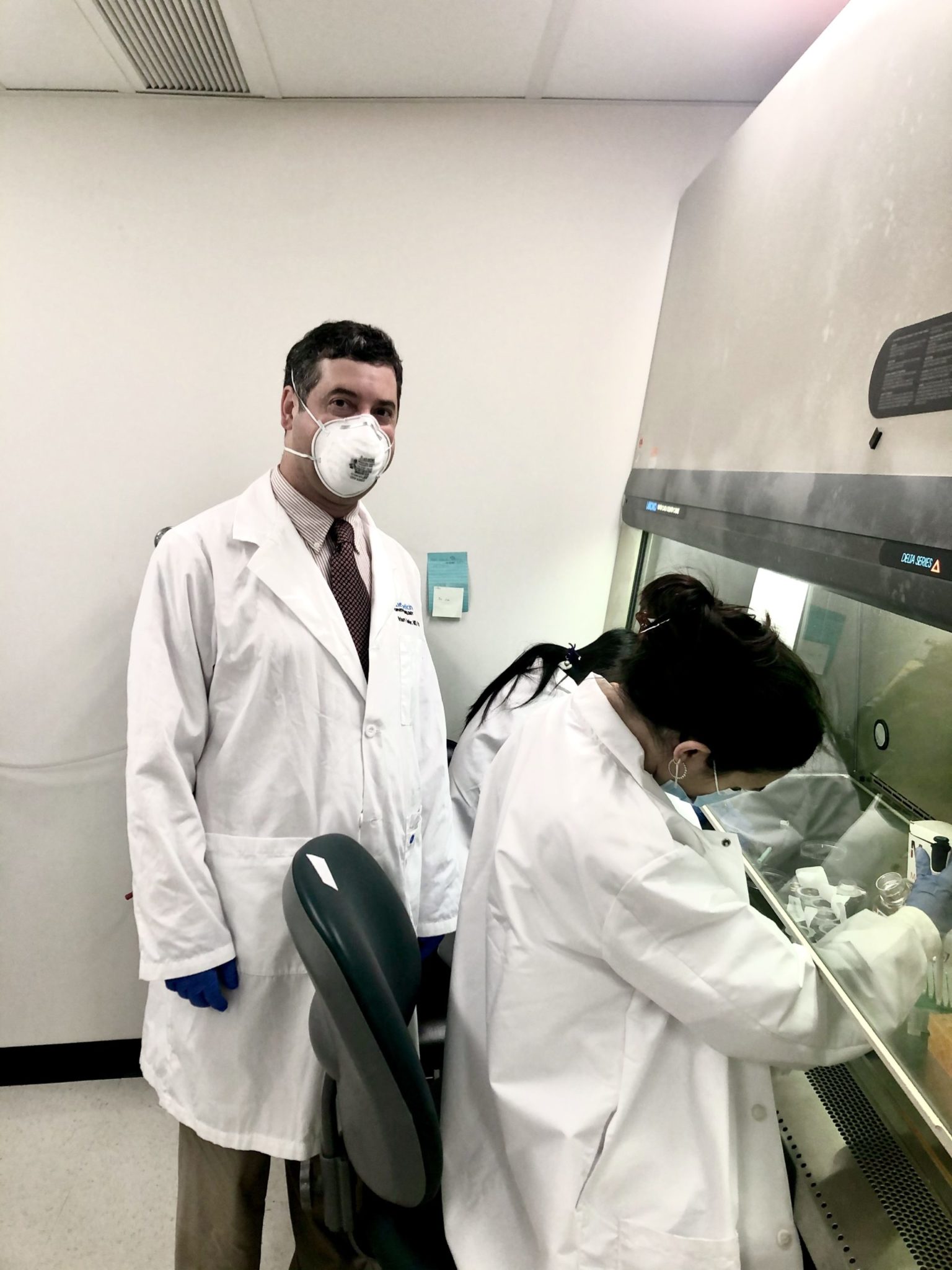
Assistant professor of Ophthalmology and Visual Science and of pathology Brian Hafler and his team have successfully sequenced the RNA of the human retina. This work has the potential to accelerate the development of treatments for conditions such age-related macular degeneration, AMD, which is a leading cause of vision loss in the world.
In October 2019, the journal Nature Communications published a study by Hafler’s team on its use of single-cell RNA sequencing to identify the cell types associated with AMD. These findings add to the 30 previously identified genes that are linked to the condition and could catalyze the development of new therapies to improve and restore vision.
“We used to think that it was the light detecting neurons that were responsible for the disease, so discovering it was actually the support cells that contained the genetic factors causing the disease was interesting,” Hafler said. “It changed the paradigm by showing us which retinal cells preferentially contribute towards degeneration, giving us a genetic context for how we should target these cell types to come up with new treatments to … prevent blindness.”
To map the RNA of the retina, the researchers employed a multi-step process involving an initial single-cell sequencing, using retina samples from six post-mortem humans. Over 20,000 cells were sequenced with a droplet-based approach, with each bead containing billions of different labels called “barcodes” and “primers,” according to Hafler.
The researchers divided the sequencing into separate batches of cells. Each time they sequenced a group of them, they used the barcodes as identification tags to keep track of which cells the information they collected came from.
The Yale scientists then collaborated with teams from the Massachusetts Institute of Technology and Harvard to complete the stage of the research that Hafler considered most challenging: using computational biology, mathematics and artificial intelligence to create algorithms to organize the raw data into a form that was suitable for interpretation. These efforts culminated in the creation of the first comprehensive human retinal genetic atlas.
Certain previously identified genes are associated with the risk of developing AMD, but this new visualization of the retina allowed the scientists to pinpoint the two specific cell types in which the aforementioned genes are expressed — glial cells, or the glue of the retina, and vascular cells that give the retina its blood supply.
“I am a little surprised that the studies suggest that microglia and vascular cells are involved early in the process of macular degeneration,” said Lucian V. Del Priore, chief of ophthalmology at Yale New Haven Hospital. “Most prior work is focused on either the retinal pigment epithelium or the photoreceptors, since early pathology is seen at this interface. Thus, Dr. Hafler‘s work is really quite groundbreaking.”
Currently, there are few ways to treat the two main types of macular degeneration, as explained in a 2019 paper by Hafler. The wet type, which is caused by the swelling of blood vessels beneath the retina, is relieved via injections that stop the blood vessels from leaking. The dry form of AMD, which is just as prevalent, can only be treated by prescribed vitamins, which are largely ineffective.
The researchers involved in Hafler’s most recent paper believe that the single-cell sequencing method they pioneered can be used to identify new pathways to treat the disease. According to Hafler, preliminary tests currently underway will determine whether blocking specific neuroinflammatory pathways can act as a new, more effective treatment.
“The potential applications of this information in clinical care would be a future direction,” said Ron Adelman, director of the Retina and Macula Service at the Yale School of Medicine, in response to questions about the Hafler Lab’s work.
Hafler conducted a not-yet-published follow-up study to expand the applications of his team’s previous findings into a clinical setting. His team compared the single-cell RNA sequencing results of human retinas with macular degeneration and glaucoma to those without, in hopes of finding differential gene expression between the two groups.
The team discovered particular pathways that are linked to disease progression and identified that macular degeneration is actually a neuroinflammatory rather than a neurodegenerative process. These findings can potentially be extrapolated to other neurodegenerative diseases, such as glaucoma.
“We found similarities between analyzing our single cell data and single cell data from Alzheimer’s disease and multiple sclerosis,” Hafler said. “They all share common paradigms across degenerative diseases. We are working on developing a common therapeutic target that we can use to treat all neurodegeneration, which includes potentially even Parkinson’s disease.”
As of 2019, more than 11 million people in the United States had some form of AMD, according to the BrightFocus Foundation.
Mai Chen | mai.chen@yale.edu







