Blumenthal, Murphy praise SalivaDirect after visiting Yale School of Public Health
Both U.S. senators expressed optimism about SalivaDirect and their eagerness to assist with scaling the testing protocol for more widespread use.
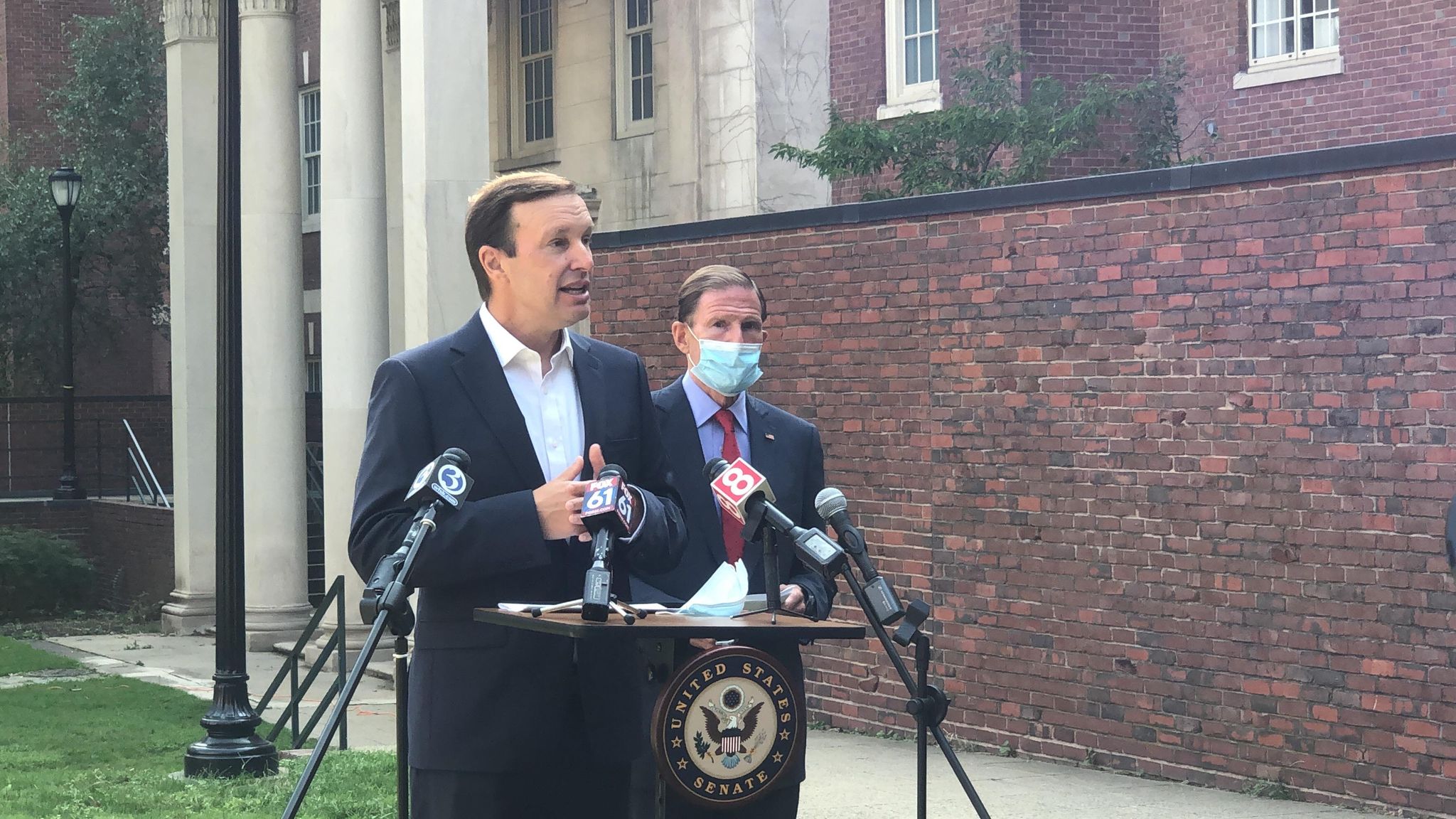
Charlotte Zimmer
Connecticut Sens. Chris Murphy and Richard Blumenthal visited the Yale medical campus Tuesday morning and met with Yale scientists to discuss SalivaDirect, the new saliva-based testing protocol developed at Yale and validated with a study funded by the NBA. Among these Yale professionals were Dean of the Yale School of Medicine Nancy Brown and Dean of the Yale School of Public Health Sten Vermund.
The initial research on using saliva samples was led by Anne Wyllie, associate research scientist in epidemiology, and Nathan Grubaugh, assistant professor of epidemiology. After obtaining promising results, they partnered with the NBA to validate the testing method on a larger cohort. The new saliva-based testing protocol received Emergency Use Authorization (EUA) from the U.S. Food and Drug Administration (FDA) on Aug. 15.
Both U.S. senators gathered on the lawn outside of Edward S. Harkness Memorial Hall after their meeting to reflect on how they envision SalivaDirect helping the state fight COVID-19.
“This test is potentially a world-shaking, really game-changing breakthrough because it can reduce the cost, raise reliability and make detection and screening much faster,” Blumenthal said. “It can produce a low cost, very sensitive and very reliable kind of test that offers, right now, massive potential results for the country.”
Blumental and Murphy applauded Yale researchers for committing to keep SalivaDirect inexpensive. After the protocol received EAU from the FDA earlier this month, Wyllie told the News that they sought to provide each test for $10 or less. A preprint published in early August estimated that the cost of reagents for each test would fall between $1.29 and $4.37 per sample.

“Right now we have a set of reagents and instruments that have been included in the EUA,” postdoctoral fellow Chantal Vogels, who helped lead the EUA submission for the FDA, told the News last week. “By performing bridging studies, we can include other reagents, instruments [and] automated systems. We just have to show that that works equally well as compared to the components that we’ve already included and have authorized.”
According to Vogels, the team is also planning on conducting bridging studies — supplemental studies that collect new data to expand the scope of the initial authorization — and working to identify equipment that other laboratories would find convenient and cost-effective for administering SalivaDirect. By identifying which bridging studies to conduct, the research team can validate the protocol with new instruments before submitting data to the FDA and seeking official approval to authorize a wider range of instrumentation for the protocol.
Running a test according to this protocol will be much cheaper than the currently available tests kits that can cost around $150, according to Wyllie. Murphy emphasized that making testing more affordable will be the key to ending this pandemic and the damage it has caused.
“There’s no amount of economic stimulus that Congress can provide to fix what’s broken in our economy, unless we beat the virus,” Sen. Murphy said. “And the only way you can beat this virus is to be doing ten to a hundred times more testing than we are today.”
Murphy expressed frustration with the country’s inability to conduct population testing, but said he is “really grateful” to Yale researchers who are studying how to address testing shortages and lower the costs of testing. According to Murphy, tests are currently too expensive or hard to acquire, and businesses and schools in New Haven could have difficulties testing all essential workers and students. Large-scale population testing would help Connecticut reopen schools and the economy with more confidence, he said.
The senators both discussed what their role would be in the next steps of developing SalivaDirect.
“Our job now is to make it available to as many people as possible, as quickly as possible,” Sen. Blumenthal said. “And I think that my goal will be to enable that it be rolled out, scaled up [and] the intellectual property protected in a way that prevents a medical device company from profiting and exploiting this test, raising the price to put it out of reach from school systems or sports leagues…”

Researchers have already been addressing the challenge of disseminating the test. Unlike other testing kits that companies sell or distribute, SalivaDirect is the first testing protocol to receive an EUA from the FDA. The protocol is open source, and researchers at Yale have the right to authorize high-complexity U.S.-based labs seeking to begin testing with SalivaDirect, though any lab that receives approval must be certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA).
Although the team initially directed requests to an email address, researchers have now set up a Google Form to field authorization requests. Hundreds of emailed requests came in the 72 hours following the announcement of SalivaDirect’s EUA, Annie Watkins MPH ’21 told the News last week.
The Yale Pathology Clinical Molecular Diagnostic Lab was the first to receive approval to use SalivaDirect, earning authorization as part of the terms of the FDA EUA. According to Pei Hui, the director of the lab, his group partnered with Grubaugh and Wyllie’s team early on to carry out the clinical validation of the testing protocol necessary for the EUA, which is something the epidemiology researchers could not do on their own.
Hui said the lab first officially started using the protocol on Thursday, Aug. 20 and added that the approval of the Yale Pathology Clinical Molecular Diagnostic Lab for SalivaDirect is a step in the right direction when it comes to scaling up the test.
“This is beauty. This is really significant progress in my view,” Hui said. “Being able to do saliva, the value is tremendous. I think it will be changing the COVID testing landscape in the US.”
The lab had already been testing nasopharyngeal swabs throughout the pandemic. Hui said they expect to maintain this testing platform as they begin to incorporate saliva samples.

He explained that his lab is currently “limited in space and manpower,” but that they hope to expand the operation. His lab will potentially buy automatic machines and use lab space at West Campus, although this would likely take a few months to set up, Hui added.
The researchers involved in SalivaDirect also contacted the Yale Testing and Tracing Committee to propose that saliva samples could potentially be used in testing the Yale community in the future, according to Hui. Both senators expressed excitement about the prospect of working with Yale to continue scaling SalivaDirect and its use.
“It is a source of enormous pride,” Blumenthal said. “I’m going to be bragging to my colleagues down in Washington about the kind of test we developed here … There is no pharmaceutical company that should profit; no medical device company should make money from it. The benefits should go directly to the public.”
William McCormack | william.mccormack@yale.edu
Charlotte Zimmer | charlotte.zimmer@yale.edu







