Joy Lian
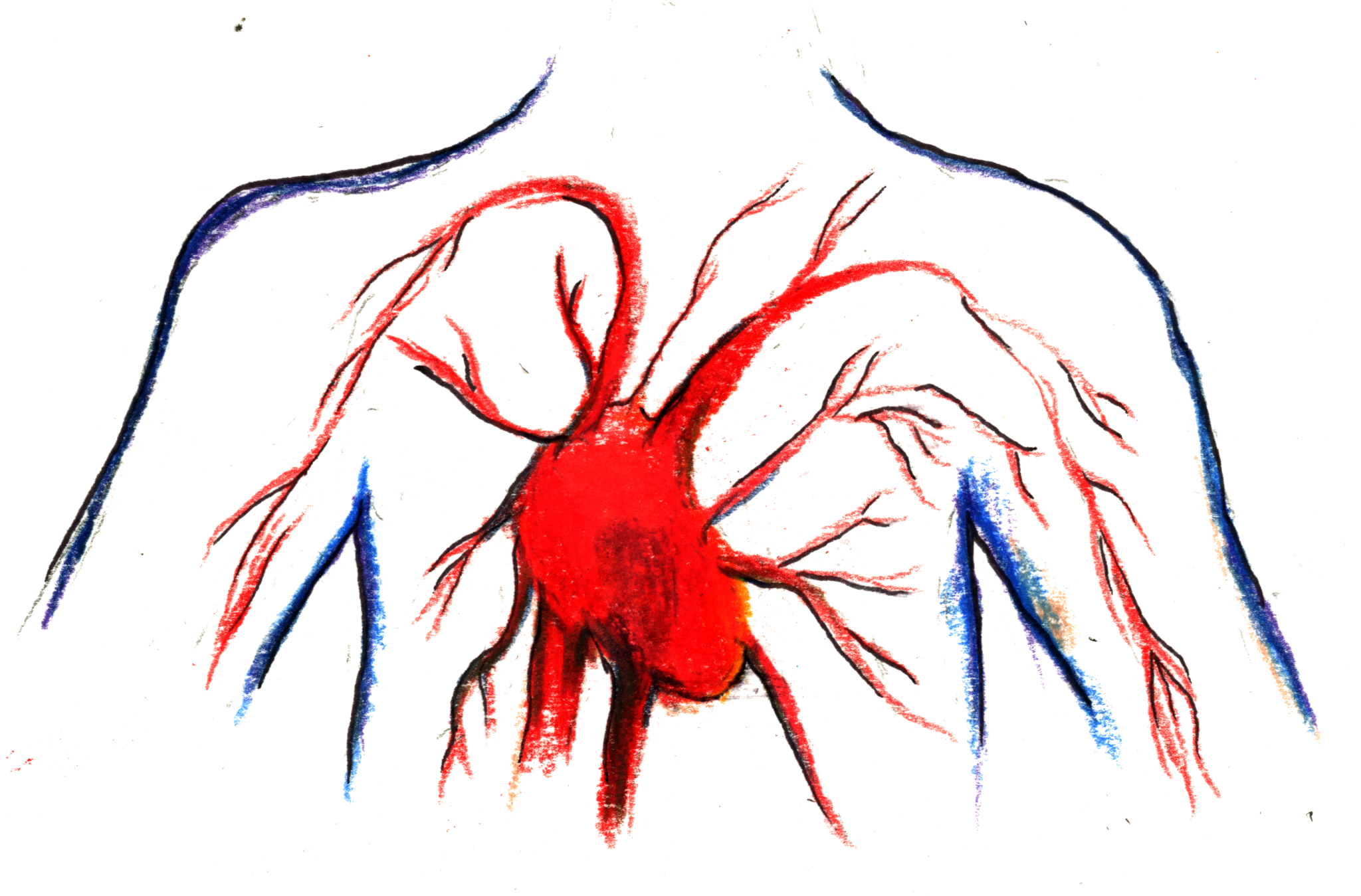
Researchers at Yale and North Carolina-based biotechnology and regenerative medicine company Humacyte have confirmed that their bioengineered blood vessels evolve into living tissue in patients, effectively carrying out the same functions as the patients’ own blood vessels.
Laura Niklason, professor of anesthesiology and biomedical engineering at the School of Medicine, led the creation of these vessels, called human acellular vessels, aiming to reduce complications in patients who depend on traditional Teflon vascular grafts — vessels that are implanted to redirect blood flow by reconnecting blood vessels.
These human acellular vessels are made by first putting human vascular cells into a biodegradable mesh scaffold in a bioreactor system, allowing for the cells to synthesize an extracellular matrix, then removing the donor cells from the system, a process called decellularization.
Prior studies have shown that about 30-40 percent of Teflon grafts fail within a year and have to be replaced. These traditional grafts — used in patients with cardiovascular or renal disease for hemodialysis, or the filtering of excess toxins from the blood — bear the risk of mechanical degradation. The body can also reject the graft, since its immune system may perceive the plastic material as a foreign invader.
“When the grafts fail, patients have to rehospitalized and it creates a lot of misery and high costs for patients,” Niklason said.
However, Niklason Lab’s new bioengineered blood vessels showed no evidence of immune rejection, according to the study.
Niklason explained that constructing rejection-free vessels was possible due to careful removal of donor cells from the graft vessel, leaving behind only the extracellular matrix, or proteins that provide support for surrounding cells.
Removing the donor cells, which makes the vessel “acellular,” reduces the risk of the immune system attacking the graft as a foreign body since the graft no longer contains donor cells containing features that are different from the host body’s cells. The extracellular matrix of human vascular tissue does not vary widely among different individuals, and the immune system is more likely to perceive the graft as “self”.
“With the highly similar extracellular matrix, it means that when these vessels are put into the body, the cells readily crawl into it, like the way people might move into empty uninhabited areas,” Niklason elaborated.
Functional tissue recellularization has the potential to enhance long-term efficacy and safety of grafts, according to Heather Prichard, co-author of the paper and chief operations officer of Humacyte.
In their publication, the team of researchers also provided a detailed characterization of the differences between the cells that migrate into the graft vessel and the cells that support the vessel by lining its microvasculature — a network of microvessels and capillaries that support the vessel.
According to Niklason, the cells that migrate into the graft vessel are highly mature, as evidenced by the proteins expressed on their membranes, or “markers,” that are typically only found in mature cells. However, the cells lining the microvessels that support the graft vessel were found to be less mature, or less differentiated, since these cells do not express the same markers. Thus, the cells of the microvessels are less specialized than the cells that migrate to the graft vessel.
According to Niklason, clinical trials using these bioengineered vessels were performed in partnership with at least 50 different medical centers in six different countries, including four European countries and Israel. The application of the vessels in multiple clinical settings will make the study more robust, she said. Currently, the vessels are in phase 3 of the clinical trial process, which is the final phase before eligibility for FDA approval.
“In our first trial, we noticed a success rate of 90 percent at one year following the [human acellular vessel] graft, as opposed to the 60-70 percent success rate for Teflon. We are hoping that Phase 3 trials will have similar results,” Niklason said.
The success of Niklason’s bioengineered blood vessels could have tremendous clinical implications upon FDA approval, according to the study. Patients with renal failure may no longer require frequent graft replacement for dialysis. In addition, patients requiring bypass, or redirection of blood flow through reconnecting blood vessels, could be treated without the need to undergo surgically invasive blood vessel harvesting.
Niklason said that she first became interested in bioengineering blood vessels because of the potentially harmful effects of surgically invasive blood vessel harvesting. During her anesthesiology residency, Niklason treated a patient who had to undergo numerous invasive incisions in order for surgeons to find a suitable blood vessel for her bypass surgery.
“The surgeons were unable to find suitable vessels in both of her legs and her arm, eventually requiring an incision to the abdomen to find a vessel for this procedure. I thought there had to be a better way than to undergo so much cutting and harvesting,” she said.
After more than 24 years of work on bioengineering blood vessels, Niklason and her team may have paved a way for patients to receive engineered vessels instead of requiring the arduous process of harvesting of blood vessels.
The National Institute of Health provides more than $445 million in funding each year to research in regenerative medicine and tissue engineering.
Viola Lee | kyounga.lee@yale.edu







