A recent study published in Nature Communications sheds light for the first time on the biological mechanism that underlies bronchopulmonary dysplasia, a disorder that primarily affects premature babies.
The study, published on Oct. 27 and conducted by Vineet Bhandari, along with other researchers at Yale and Drexel universities, identifies a target molecule, microRNA-34a, involved in numerous biological pathways associated with the disease. Levels of this molecule are elevated in BPD in both mouse and human models, and Bhandari has identified multiple possible therapies related to this microRNA.
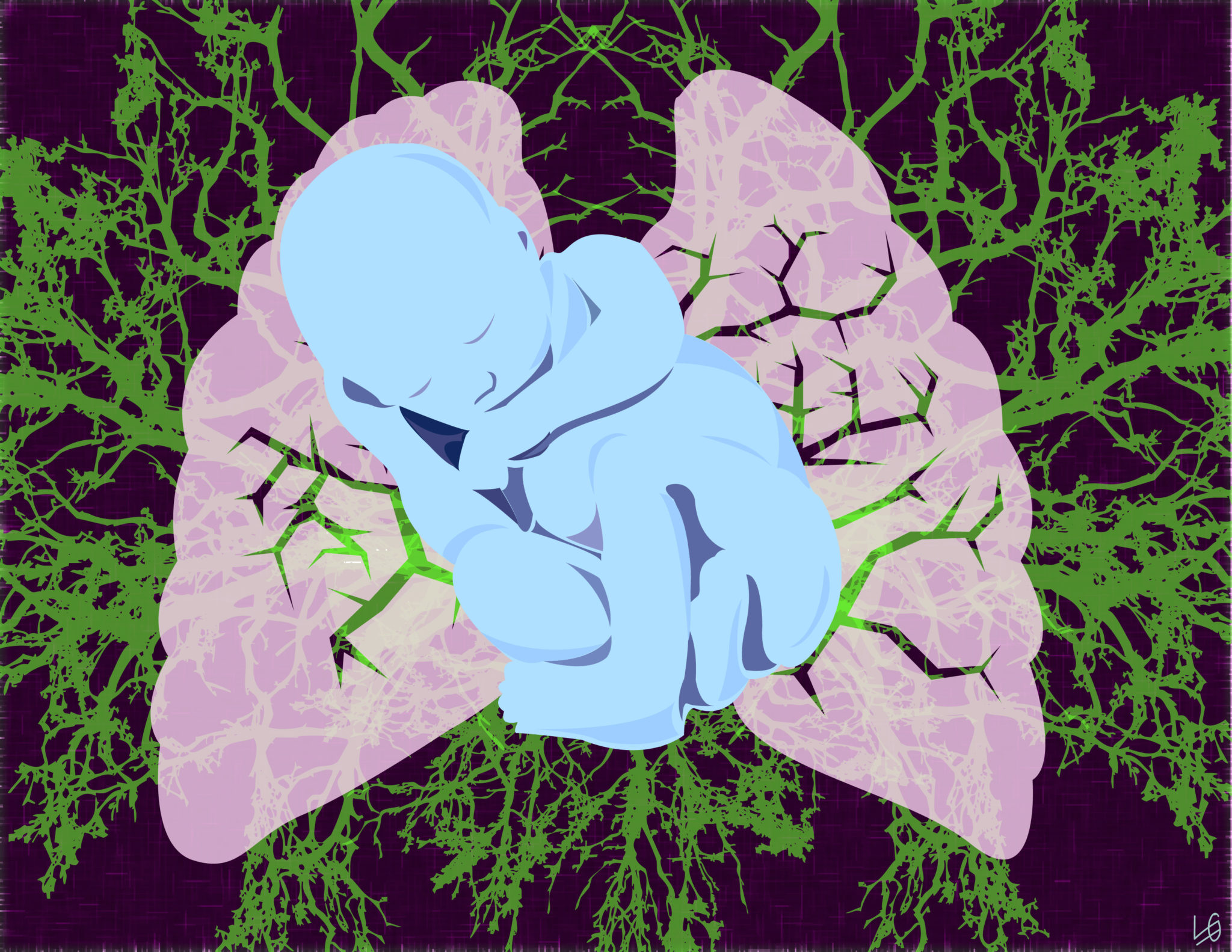
Premature babies are some of the most fragile creatures on Earth, often requiring intensive care to remain alive. For those babies who lack functional lungs, oxygen is pumped in through a ventilator, allowing their bodies to get the oxygen they need. This ventilation and excess of oxygen, however, can result in another problem: BPD, which can permanently damage the baby’s lungs.
“While neonatology has advanced tremendously in the past 20 years, we still cannot avoid the development of BPD,” said Gloria Pryhuber, a co-author of the study and a professor at the University of Rochester’s medical center. “This finding is very exciting, as it suggests a series of potential therapeutic interventions … potentially repairing and preventing the development of BPD.”
MicroRNAs are a class of biological molecules whose functions scientists did not understand until recently. Composed of around 20 RNA units, these molecules can interfere with and silence other proteins in a cell — like jamming a signal on a radio. Unlike many other molecules, which have a single purpose, microRNAs are able to control a wide variety of responses. They are signal-jammers that jam not just one radio frequency but the whole FM spectrum.
“I’ve been working on BPD for more than 25 years now, and people have said it’s too complex of a disease to have [a single cause],” said Bhandari, who was a professor at the Yale School of Medicine until 2015. “But when I started reading about these microRNAs, which can control multiple pathways, I was intrigued.”
Bhandari suspected one of these microRNAs might be responsible for the various conditions associated with BPD and, while at Yale, began screening for them in late 2013. After numerous rounds of testing, Bhandari happened upon microRNA-34a, which he found in unusually high amounts in BPD-affected lungs. His team concluded that this microRNA was able to control each of the four conditions associated with BPD — a “master regulator” of the disease most neonatal scientists thought could not exist, according to Bhandari.
And they had good reason not to. The symptoms of BPD vary widely, from a slight increase in breathing rate to complete respiratory failure, which makes the disease difficult to characterize and even harder to define. It is caused by what Bhandari calls a “perfect storm of environmental and genetic factors,” and researchers have yet to develop a therapy against the disease.
Initially skeptical of finding a “master regulator,” Bhandari has spent the past few years rigorously testing microRNA-34a to see whether it truly was what it appeared to be, performing a number of experiments in mice and in deceased babies to confirm the high presence of this molecule in BPD-related pathways. Bhandari said his team found that mice engineered with a lack of this microRNA were symptom-free, seemingly unable to develop BPD. Most importantly, when Bhandari lowered the level of microRNA-34a in mice that already had BPD, the symptoms of the disease stopped worsening and even began to reverse.
This last finding strongly suggests that targeting microRNA-34a could be the key to creating the first-ever medically approved therapy for infants with the disease, a huge stride forward for the neonatal research community, Bhandari said. He added that his team has already developed a drug that inhibits the microRNA. The team plans on incorporating the drug into established care routines for premature babies.
BPD, the most common infant lung disease, has the potential to affect around 10,000 newborns each year in the United States.
Conor Johnson | conor.johnson@yale.edu







